Type 2 diabetes is a prevalent and progressive metabolic disorder that affects millions of people worldwide. Understanding how type 2 diabetes progresses, the factors contributing to its development, and the transition from prediabetes to diabetes is crucial for effective prevention and management. In this article, we’ll delve into the progression of type 2 diabetes, the key factors involved, and what you need to know about the transition from prediabetes to diabetes, as well as prevention and management strategies.
Progression of Type 2 Diabetes
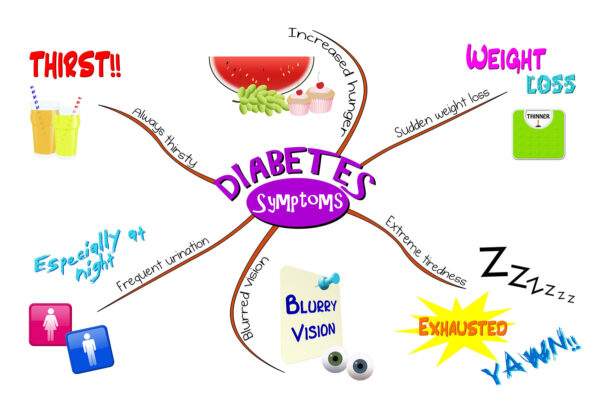
- Insulin Resistance: The early stage of type 2 diabetes is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin. This requires the pancreas to produce more insulin to maintain normal blood sugar levels.
- Prediabetes: Before the diagnosis of type 2 diabetes, individuals often experience prediabetes, a condition where blood sugar levels are higher than normal but not yet in the diabetes range. Prediabetes serves as a warning sign and an opportunity for intervention.
- Beta Cell Function Decline: Over time, the insulin-producing beta cells in the pancreas may gradually lose their ability to produce sufficient insulin. This contributes to the progression of type 2 diabetes.
- Diabetes Diagnosis: When blood sugar levels consistently remain elevated and meet diagnostic criteria, a diagnosis of type 2 diabetes is made. This diagnosis marks the transition from prediabetes to diabetes.
Factors Influencing Progression
Several factors can influence the progression of type 2 diabetes:
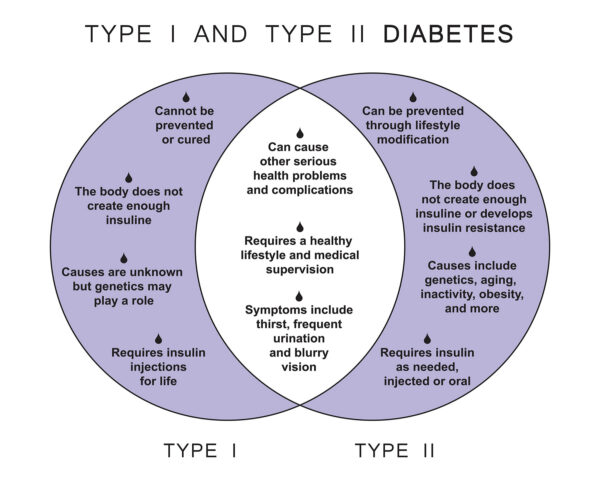
- Genetics: Family history and genetic predisposition play a role in diabetes development.
- Lifestyle: Sedentary behavior, poor dietary choices, excess body weight, and lack of physical activity can accelerate the progression.
- Age: The risk of type 2 diabetes increases with age, but it can affect people of all age groups.
- Medical Conditions: Certain medical conditions, such as high blood pressure and high cholesterol, can contribute to diabetes progression.
Transition from Prediabetes to Diabetes
The transition from prediabetes to type 2 diabetes can be gradual, and it may not always be noticeable. It underscores the importance of regular healthcare check-ups and monitoring of blood sugar levels. Lifestyle changes, such as adopting a balanced diet, increasing physical activity, and maintaining a healthy weight, can help delay or prevent this transition.
Prevention and Management Strategies
- Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit sugar and processed foods.
- Physical Activity: Engage in regular physical activity, including aerobic exercise and strength training, to improve insulin sensitivity.
- Weight Management: Achieving and maintaining a healthy weight can significantly reduce the risk of diabetes and slow its progression.
- Medication and Insulin: When necessary, healthcare providers may prescribe medications or insulin to help control blood sugar levels.
- Regular Monitoring: Keep track of blood sugar levels as recommended by a healthcare provider. This helps identify changes and adjust treatment plans accordingly.
- Lifestyle Modifications: Make sustainable lifestyle changes, including quitting smoking and managing stress, to support overall health.
Proactive Measures for Diabetes Control
Understanding the progression of type 2 diabetes and the transition from prediabetes to diabetes empowers individuals to take proactive measures for prevention and control. By embracing a healthy lifestyle, regular monitoring, and medical guidance, it is possible to slow the progression of type 2 diabetes and enjoy improved overall well-being. Early intervention and consistent management are key factors in effectively managing type 2 diabetes.