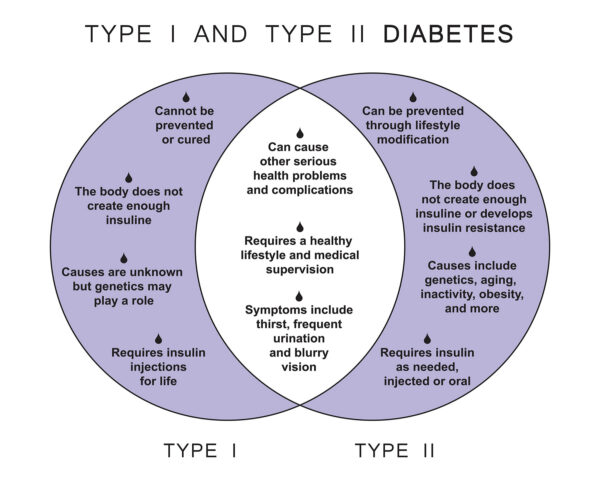
Diabetes is a complex condition with various forms, but the two most prevalent types are type 1 and type 2 diabetes. Understanding the key differences between these two types is essential for individuals living with diabetes and their healthcare providers. In this article, we will decipher the critical distinctions between type 1 and type 2 diabetes, encompassing their causes, symptoms, treatments, and management strategies.
1. Causes and Autoimmunity
- Type 1 Diabetes: This form of diabetes is primarily caused by an autoimmune response in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. The exact cause of this autoimmune response is not fully understood, but genetics and environmental factors may play a role.
- Type 2 Diabetes: Type 2 diabetes typically develops due to insulin resistance, where the body’s cells do not respond effectively to insulin, and the pancreas may not produce enough insulin. Genetics, family history, and lifestyle factors such as poor diet and sedentary behavior contribute to type 2 diabetes.
2. Age of Onset
- Type 1 Diabetes: It is often diagnosed in childhood or adolescence, although it can occur at any age. It accounts for a smaller percentage of diabetes cases.
- Type 2 Diabetes: Type 2 diabetes is more commonly diagnosed in adulthood, but it can also develop in children and adolescents. It represents the majority of diabetes cases worldwide.
3. Insulin Dependency
- Type 1 Diabetes: Individuals with type 1 diabetes are entirely dependent on insulin therapy for survival. They require insulin injections or insulin pump therapy to manage their blood sugar levels.
- Type 2 Diabetes: While many people with type 2 diabetes may initially manage their condition with lifestyle changes, some may eventually require oral medications, injectable medications, or insulin to control blood sugar.
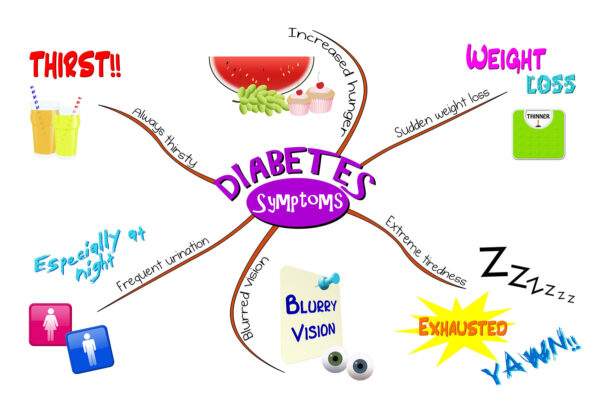
4. Symptoms
- Type 1 Diabetes: Symptoms of type 1 diabetes often develop quickly and may include excessive thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
- Type 2 Diabetes: Symptoms of type 2 diabetes may develop gradually and can include frequent urination, increased thirst, fatigue, slow wound healing, and recurring infections.
5. Body Weight and Body Mass Index (BMI)
- Type 1 Diabetes: It is not associated with body weight or BMI, as it is primarily an autoimmune condition.
- Type 2 Diabetes: Type 2 diabetes is often linked to excess body weight and higher BMI. However, it can also occur in individuals with normal or lower BMI.
6. Treatment and Management
- Type 1 Diabetes: Management of type 1 diabetes focuses on insulin therapy, blood sugar monitoring, and careful meal planning. Advanced technologies like insulin pumps and continuous glucose monitoring systems offer precise control.
- Type 2 Diabetes: Treatment for type 2 diabetes includes lifestyle modifications such as diet and exercise, oral medications, injectable medications, and insulin therapy when necessary. Weight management and regular blood sugar monitoring are crucial components.
7. Risk Factors for Complications
- Type 1 Diabetes: Individuals with type 1 diabetes are at risk for complications such as neuropathy, retinopathy, and kidney disease if blood sugar levels are not well-controlled.
- Type 2 Diabetes: Type 2 diabetes is often associated with obesity and is a major risk factor for complications, including heart disease, stroke, kidney disease, and eye problems.
Understanding Diabetes Types for Better Management
Deciphering the differences between type 1 and type 2 diabetes is vital for individuals and healthcare providers alike. By recognizing the causes, symptoms, and treatment approaches specific to each type, individuals with diabetes can tailor their management strategies to achieve better blood sugar control and overall well-being. Regardless of the type of diabetes, early diagnosis, appropriate treatment, and a healthy lifestyle play pivotal roles in effective diabetes management.