Misinformation and myths often surround chronic health conditions like diabetes. These misconceptions can lead to confusion and, in some cases, hinder effective diabetes management. It’s essential to separate fact from fiction when it comes to diabetes to make informed decisions about your health. In this article, we’ll debunk common diabetes myths and provide you with the knowledge needed to distinguish between myths and realities for better diabetes management.
Myth #1: Diabetes Is Only Caused by Eating Too Much Sugar
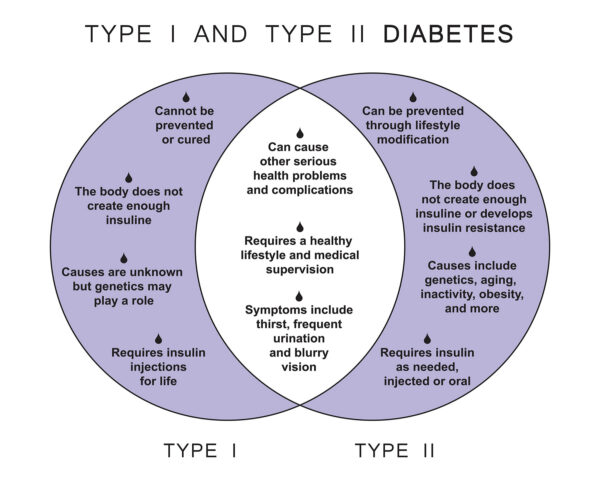
Reality: While excessive sugar consumption can contribute to the development of type 2 diabetes, it is not the sole cause. Genetics, family history, lifestyle factors, and insulin resistance also play significant roles in diabetes onset. Managing diabetes involves more than just reducing sugar intake; it requires a comprehensive approach to diet, exercise, and healthcare.
Myth #2: People with Diabetes Should Avoid All Carbohydrates
Reality: Carbohydrates are a primary source of energy and should be part of a balanced diet for people with diabetes. The key is to choose complex carbohydrates like whole grains, fruits, and vegetables, which have a more gradual impact on blood sugar levels. Portion control and monitoring carbohydrate intake are essential for effective diabetes management.
Myth #3: People with Diabetes Can’t Enjoy Sweets or Desserts
Reality: People with diabetes can enjoy sweets and desserts in moderation. The key is to incorporate them into a well-balanced meal plan and monitor blood sugar levels carefully. Sugar-free and low-sugar alternatives are available for many sweet treats, providing options for those with diabetes.
Myth #4: Insulin Is a Last Resort for Diabetes Treatment
Reality: Insulin is a valuable and often necessary treatment for people with diabetes, especially for those with type 1 diabetes. It can also be used in combination with other medications for type 2 diabetes. Insulin therapy is not a sign of failure but rather a crucial tool for achieving and maintaining target blood sugar levels.
Myth #5: Only Overweight People Get Diabetes
Reality: While obesity is a risk factor for type 2 diabetes, diabetes can affect individuals of all body types. Genetics, family history, and other factors play a significant role in diabetes development. It’s essential to focus on overall health and risk factors rather than making assumptions based on weight alone.
Myth #6: Diabetes Is Contagious
Reality: Diabetes is not contagious and cannot be spread from person to person. It is a metabolic disorder that results from a combination of genetic and environmental factors. You cannot “catch” diabetes from someone who has it.
Myth #7: People with Diabetes Should Only Eat “Diabetic” Foods
Reality: “Diabetic” foods are not necessary for diabetes management and can sometimes be misleading. Many so-called diabetic foods may still affect blood sugar levels. It’s more important to focus on a balanced diet that includes a variety of nutrient-rich foods.
Myth #8: You Can Outgrow Diabetes
Reality: While type 2 diabetes can sometimes be managed effectively with lifestyle changes, it does not typically go away entirely. It may go into remission, but ongoing monitoring and healthcare are essential to prevent relapse.
Myth #9: Diabetes Always Leads to Severe Complications
Reality: With proper management, diabetes-related complications can be reduced or prevented. Regular monitoring, medication adherence, a healthy lifestyle, and timely medical care are key factors in reducing the risk of complications.
Myth #10: You Can Stop Taking Medications Once Your Blood Sugar Is Normal
Reality: Medications prescribed for diabetes should not be discontinued without consulting a healthcare provider. Even when blood sugar levels are well-controlled, medications may still be necessary to maintain stability.
Conclusion: Knowledge Empowers Effective Diabetes Management
Debunking common diabetes myths is essential for accurate information and effective diabetes management. Understanding the realities of diabetes helps individuals make informed choices about their diet, lifestyle, and healthcare. It’s important to consult with a healthcare provider or diabetes educator for personalized guidance and to address any specific concerns related to diabetes management.