The Importance of Foot Care in Diabetes
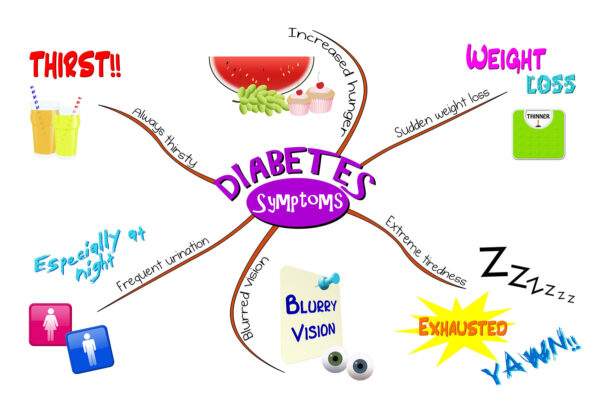
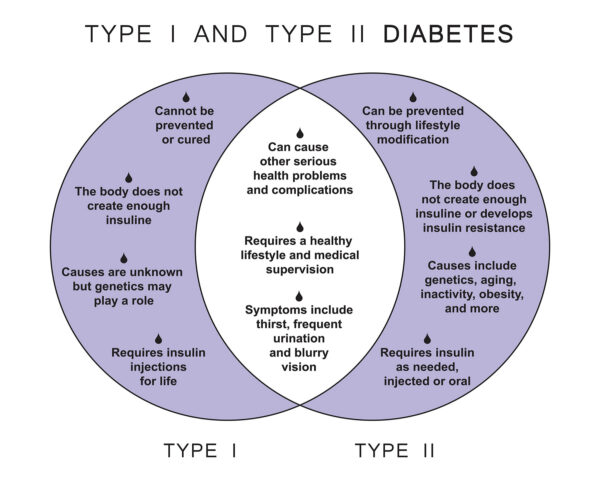
Foot care is a critical aspect of diabetes management. Due to the risk of neuropathy and poor circulation associated with diabetes, choosing the right footwear, including insoles, is crucial for preventing foot complications.
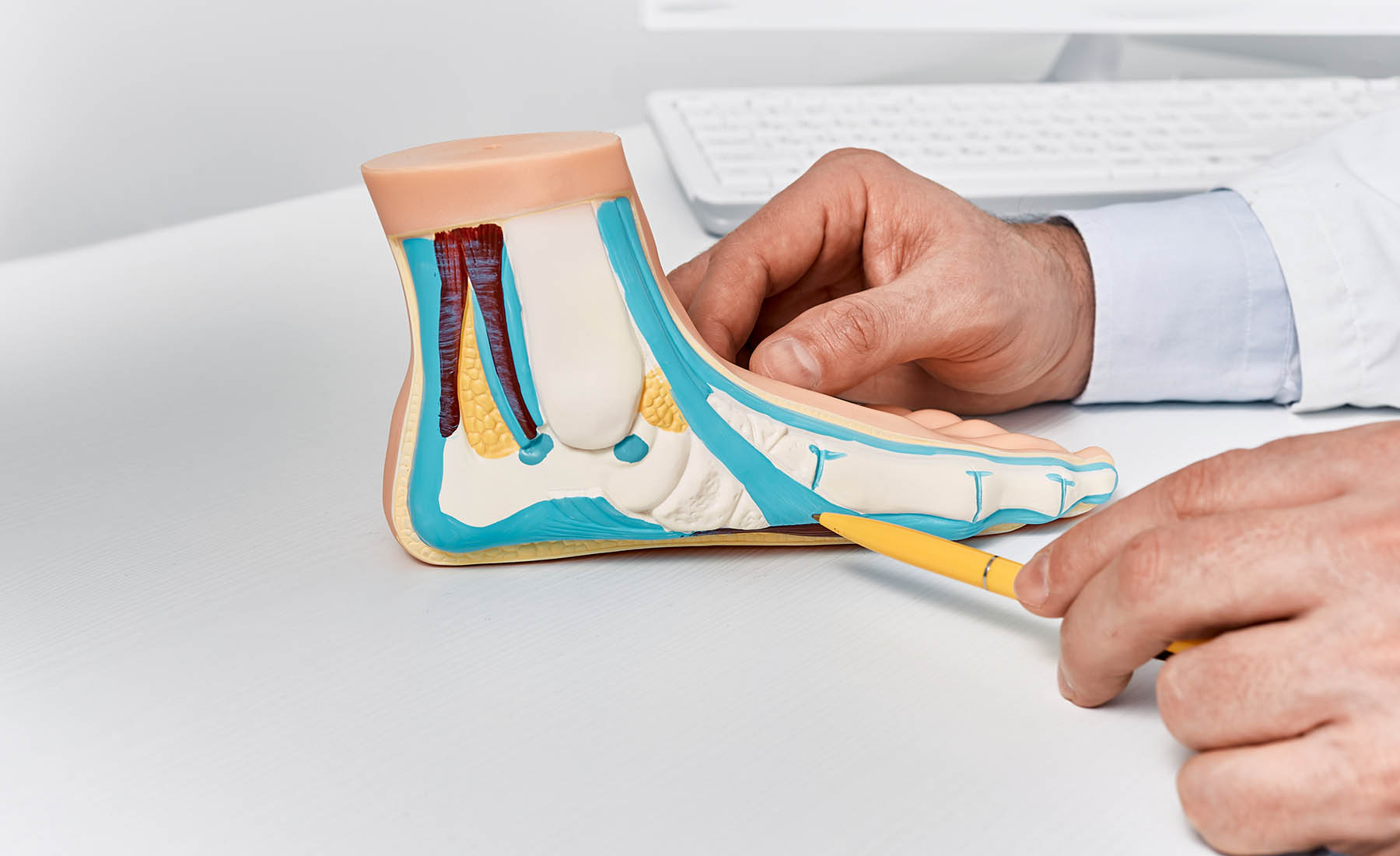
Understanding Diabetic Insoles
Diabetic insoles are designed to provide extra support, reduce pressure points, and improve comfort. They play a vital role in preventing foot injuries and complications, a common concern for individuals with diabetes.
Features of Diabetic Insoles
Quality diabetic insoles typically feature:
- Soft, cushioning materials that reduce impact and pressure
- Arch support to distribute weight evenly
- Non-irritating seams to prevent rubbing and blisters
- Heat-retention properties for improved blood circulation
Choosing the Right Diabetic Insoles
When selecting diabetic insoles, consider:
- The material: Look for breathable, moisture-wicking materials.
- The fit: Ensure they fit well in your shoes without being too tight.
- Customization: Custom-made insoles can provide tailored support and comfort.
The Role of Insoles in Preventing Diabetic Foot Complications
Diabetic insoles help in reducing the risk of foot ulcers and other complications by evenly distributing pressure, minimizing friction, and providing additional cushioning.
Integrating Diabetic Insoles into Daily Life
Integrate diabetic insoles into your daily routine for maximum benefit. Wear them in your everyday shoes, and particularly in shoes you wear for extended periods, like work shoes or walking shoes.
Regular Inspection and Replacement
Regularly inspect your insoles for signs of wear and tear. Replace them as needed to ensure continuous foot protection and support. Insoles, like any other part of your diabetic foot care routine, require ongoing attention.
Additional Diabetic Foot Care Tips
In addition to using diabetic insoles, maintain a comprehensive foot care regimen:
- Conduct daily foot inspections for cuts, blisters, or sores.
- Keep your feet clean and moisturized.
- Trim toenails straight across to avoid ingrown nails.
- Wear well-fitting, comfortable shoes.
Consulting with Healthcare Professionals
Consult with healthcare professionals, such as a podiatrist, for recommendations on diabetic insoles and overall foot care strategies. They can provide advice tailored to your specific needs and conditions.
Stepping Towards Better Health
Investing in diabetic insoles is a step towards maintaining healthy feet as a diabetic. They offer the necessary support and comfort, reducing the risk of foot complications and contributing to overall well-being and mobility.